[Webinar Summary] Rx Hand Hygiene: Facilitating Clean Hands in Healthcare Facilities During COVID-19 and Beyond
May 8, 2020
On May 7, 2020 at 8am EDT (12pm UTC), the Global Handwashing Partnership and Emory University’s Center for Global Safe Water, Sanitation and Hygiene (WASH) hosted a webinar highlighting the importance of access to hand hygiene facilities and practical actions that can be taken in low-resource settings.
COVID-19 has amplified the importance of proper hand hygiene in healthcare settings. Similarly, Hand Hygiene Day and International Day of the Midwife – both commemorated on May 5 – emphasize the role hand hygiene plays in delivering safe and clean care. Webinar objectives included:
- Discuss the role of hand hygiene and other IPC measures in healthcare facilities for disease prevention
- Address issues of hand recontamination in a healthcare setting; and
- Share experiences and solutions to increase access to hand hygiene facilities
Ron Clemmer and Aarin Palomares from the Global Handwashing Partnership were moderators for the webinar, while Lindsay Denny from the Emory University Center for Global Safe Water, Sanitation, and Hygiene provided closing remarks. Presentation slides and key resources can be found here.
Summary of Presentations
Julie Storr and Claire Kilpatrick, both consultants to WHO, introduced the need for hand hygiene in healthcare facilities and key messages to convey. The WHO’s multimodal improvement strategy can improve hand hygiene by applying a series of steps, detailed here. Additional hand hygiene resources can be found here.
Dr. Benjamin Park, Chief of the International Infection Prevention Program at CDC, then provided context of infection and prevention control (IPC) for COVID-19 to support the maintenance of essential healthcare services by preventing healthcare-associated transmission of SARS-CoV-2 among healthcare workers and patients. Steps for limiting unrecognized entry of COVID-19 include triaging patients, limiting visitors, and monitoring staff. Likewise, training staff and ensuring access to supplies, including hand hygiene facilities for patients upon arrival, can help to prevent transmission. Rapidly identifying nosocomial transmission is needed to contain outbreaks before they spread. Operational considerations, including hand hygiene guidance, can be found here. The CDC will be launching a COVID-19 IPC webinar series, tentatively starting on May 12. Follow @CDCgov online for more information.
Dr. Matthew Lozier, a Lieutenant Commander with the US Public Health Service and Epidemiologist at CDC, followed up with practical actions to increase access to hand hygiene resources, providing a case study from a program in Uganda. To support hand hygiene, it is important to conduct a rapid assessment to identify gaps in hand hygiene resources and determine the best strategy to address these gaps. Hand hygiene resources are needed in critical points of care, points of entry, and near latrines (see slide below). Conveniently located handwashing resources with soap and water can make individuals 80% more likely to practice handwashing. Handwashing stations should be user-friendly, durable, and provide an area for soap. Specific staff should be responsible for upkeep of handwashing stations as part of their jobs.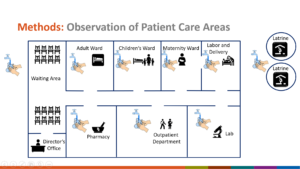
Alcohol-based handrub (ABHR) is a necessary part of a hand hygiene regimen in a health facility. Dr. Lozier then discussed their program in Uganda to produce ABHR for local distribution and use through district-based production following the ethonal-based WHO formulation. The program resulted in a significant increase in hand hygiene adherence among healthcare workers. Key considerations for such a program include close collaboration with partners, quality control, packaging, distribution, and accounting for the local context. More on the program can be found here.
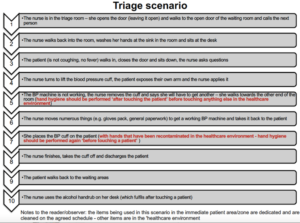
Dr. Giorgia Gon, Assistant Professor for the London School of Hygiene and Tropical Medicine, addressed hand and glove recontamination. Her research addresses hand hygiene compliance in labor and delivery wards in Tanzania, examining re-contamination occurrences as part of a time-and-motion study. As part of the methodology, observers were asked to write down each action birth attendants took 24 hours per day, 6 days a week. Results showed that recontamination happened when touching the following surfaces: glove packs, PPE, patients outside the patient zone, and personal bags. An example of hand recontamination during a triage event can be seen in image below.
Panel Discussion
Following the technical presentations, a panel of experts convened to dive deeper into practical hand hygiene solutions. Panelists included:
- Tom Bergin, Healthcare Marketing Director, Essity Professional Hygiene
- Geoff Revell, Founder and Managing Director, HappyTap
- Stuart Mason, CEO and Inventor, SPATAP Portable Tap
- Pavani Ram, Senior Medical Advisor, USAID
Innovative solutions for access
HappyTap and SPATAP provide handwashing solutions that are portable, durable, and water-efficient. Both handwashing station products can be deployed rapidly and do not rely on a piped water supply. Compendiums developed by UNICEF and IDS list other handwashing facility solutions for COVID-19. A low-cost handwashing station is a good immediate solution, but it is also important to find the balance of these low-cost solutions and provision of long-term WASH infrastructure.
The importance of handwashing station design and placement
The rates of consistent handwashing practice is based on the location of a handwashing station. The more convenient a facility is, the more likely a person is to wash their hands. For portable stations like HappyTap and SPATAP, their size may be an advantage to allow for more handwashing stations to comply with social distancing at this time. Additionally, the portable nature of these products allow a healthcare facility to have multiple stations at critical points in the facility.
Essity developed a placement guide for alcohol-based handrub dispensers since optimizing dispenser placement can increase usage by 50%. Dispensers should be placed at primary points of care and high traffic routes. Find the dispenser guide and other materials here.
IPC and WASH Coordination
Leadership must be motivated to accomplish hand hygiene in healthcare facilities. During the COVID-19 outbreak, hand hygiene and other safety measures are in most health workers minds. It is important to have a designated person responsible for ensuring the hand hygiene program is properly maintained and used. Having supplies at the healthcare facility is not enough; there must be someone to advocate and train staff, while ensuring supplies are constantly available at critical locations. This requires someone with training in IPC to ensure that the pandemic does not result in degrading provision of safe care. The importance of WASH in a healthcare facility is critical to support IPC.
Sustaining handwashing behavior change beyond the crisis
With any time of crisis, there is a need to think of resilience. To enact lasting change, this requires changes in policies and funding at the highest levels. Documentation and the development of a convincing argument that WASH infrastructure is critical for the provision of safe care is required. There is no better time than now. Also, addressing recontamination is rarely prominent in trainings and guidelines, and it is essential to accomplish acceptable hand hygiene. While COVID-19 provides an opportunity to highlight the importance of a hand hygiene, we must be vigilant and not forget the need to prioritize hand hygiene long-term.